Contraception and Family Planning Terms: Your Complete Reference Guide
Understand contraception and family planning terminology with clear definitions of birth control methods, fertility concepts, and reproductive health terms.

Contraception and family planning represent fundamental aspects of reproductive health that affect millions of people worldwide. Understanding the terminology used in these fields empowers individuals to make informed decisions about their reproductive choices, communicate effectively with healthcare providers, and access appropriate services and information. This comprehensive reference guide provides clear, accurate definitions of contraceptive methods, fertility concepts, and family planning terminology while acknowledging the diverse needs and circumstances that influence reproductive decision-making.
Basic Contraception Concepts
Fundamental Definitions
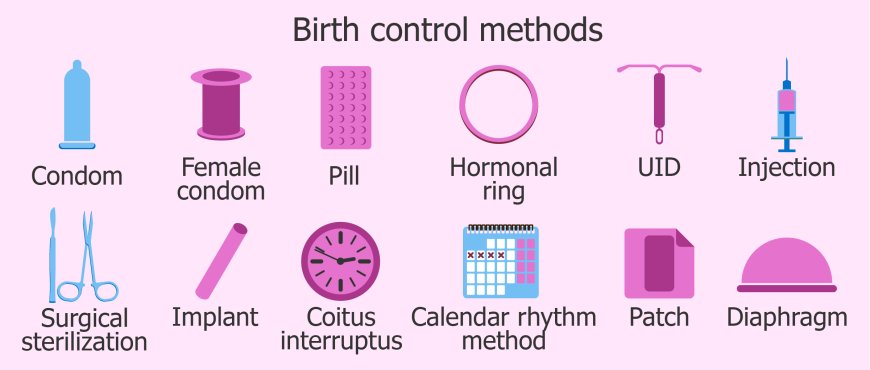
Contraception refers to methods or devices used to prevent pregnancy during sexual intercourse. Also known as birth control, contraception encompasses a wide range of approaches that work through different mechanisms to reduce the likelihood of conception.
Family planning is the broader concept of making informed decisions about if, when, and how many children to have. This includes contraception for pregnancy prevention as well as fertility treatments for those trying to conceive, and encompasses the spacing and timing of pregnancies.
Efficacy describes how well a contraceptive method works in preventing pregnancy, typically expressed as a percentage of effectiveness over one year of use. Efficacy rates are usually given for both "perfect use" (when the method is used correctly and consistently) and "typical use" (accounting for human error and inconsistent use).
Perfect use efficacy reflects how well a contraceptive method works when used exactly as directed without any errors, missed doses, or inconsistent application. These rates represent the theoretical maximum effectiveness of each method.
Typical use efficacy accounts for real-world usage patterns, including occasional missed pills, inconsistent condom use, or other human factors that may reduce effectiveness. These rates better reflect how well methods work in practice for most users.
Contraceptive failure occurs when pregnancy happens despite using a birth control method. Failure can result from method failure (the contraceptive itself doesn't work) or user failure (incorrect or inconsistent use of the method).
Hormonal Contraception
Oral Contraceptives
Birth control pills, commonly called "the pill," are oral medications containing synthetic hormones that prevent pregnancy by suppressing ovulation, thickening cervical mucus, and thinning the uterine lining. Pills must be taken daily to maintain effectiveness.
Combination pills contain both estrogen and progestin hormones and represent the most common type of oral contraceptive. These pills typically follow a 21-day active pill regimen followed by 7 days of placebo pills or no pills, during which withdrawal bleeding occurs.
Progestin-only pills, also called mini-pills, contain only synthetic progesterone and are often recommended for people who cannot take estrogen due to medical conditions or breastfeeding. These pills must be taken at the same time each day to maintain effectiveness.
Extended-cycle pills are designed to reduce the frequency of menstrual periods by extending the time between withdrawal bleeds. These formulations may provide 12 weeks of active hormones followed by one week of placebo pills, resulting in only four periods per year.
Other Hormonal Methods
The contraceptive patch is a thin, adhesive patch that releases hormones through the skin. Users apply a new patch weekly for three weeks, followed by one patch-free week during which withdrawal bleeding occurs.
The vaginal ring is a flexible ring inserted into the vagina that releases hormones locally. Users typically insert a new ring monthly, leaving it in place for three weeks and removing it for one week to allow withdrawal bleeding.
Contraceptive injections, such as Depo-Provera, provide long-acting hormonal birth control through intramuscular injections given every three months. These injections contain progestin only and may cause menstrual changes including cessation of periods.
Contraceptive implants are small, flexible rods inserted under the skin of the upper arm that release progestin over several years. Currently available implants provide contraceptive protection for up to three years and can be removed at any time to restore fertility.
Intrauterine Devices (IUDs)
Types of IUDs
Hormonal IUDs are T-shaped devices inserted into the uterus that release progestin locally over several years. These devices prevent pregnancy by thickening cervical mucus, thinning the uterine lining, and sometimes suppressing ovulation.
Copper IUDs, such as the Paragard, are non-hormonal devices that prevent pregnancy by creating an environment toxic to sperm and eggs. The copper IUD can provide contraceptive protection for up to 10 years and doesn't affect natural hormone cycles.
IUD-Related Terms
Insertion refers to the medical procedure of placing an IUD into the uterus, typically performed in a healthcare provider's office. The procedure involves opening the cervix slightly to guide the IUD through the cervical canal into the uterine cavity.
Expulsion occurs when an IUD is pushed out of the uterus by uterine contractions, which happens in approximately 2-5% of users, typically within the first few months after insertion.
Perforation is a rare complication where the IUD punctures through the uterine wall during insertion or afterward. This serious complication requires surgical removal of the device.
Barrier Methods
Male and Female Condoms
Male condoms are thin sheaths, typically made of latex, polyurethane, or polyisoprene, that cover the penis during sexual intercourse to prevent sperm from entering the vagina. Condoms also provide protection against sexually transmitted infections.
Female condoms, also called internal condoms, are pouches inserted into the vagina before sexual intercourse to prevent sperm from reaching the cervix. These condoms also provide STI protection and can be inserted up to 8 hours before intercourse.
Latex sensitivity affects people who experience allergic reactions to natural rubber latex, requiring alternative condom materials such as polyurethane, polyisoprene, or lambskin (though lambskin doesn't protect against STIs).
Other Barrier Methods
Diaphragms are shallow, dome-shaped cups made of silicone that cover the cervix to prevent sperm from entering the uterus. Diaphragms must be fitted by healthcare providers and used with spermicide for optimal effectiveness.
Cervical caps are smaller, thimble-shaped devices that fit directly over the cervix to block sperm entry. Like diaphragms, cervical caps require professional fitting and spermicide use.
Contraceptive sponges are soft, foam devices infused with spermicide that are inserted into the vagina to cover the cervix. The sponge provides contraceptive protection for 24 hours regardless of the number of sexual encounters during that time.
Spermicides and Chemical Barriers
Spermicides are chemical agents that immobilize or kill sperm, typically containing nonoxynol-9 as the active ingredient. Spermicides are available as creams, gels, foams, suppositories, and sponges.
Nonoxynol-9 is the most common spermicidal agent used in contraceptive products. However, frequent use of nonoxynol-9 can cause vaginal irritation and may increase STI transmission risk by disrupting protective vaginal tissues.
Natural Family Planning and Fertility Awareness
Fertility Awareness Methods
Natural family planning (NFP) encompasses methods that use awareness of fertility signs to either avoid or achieve pregnancy without using artificial contraceptives. These methods require education, motivation, and consistent monitoring of fertility indicators.
The calendar method involves tracking menstrual cycles over several months to predict fertile days based on cycle length patterns. This method is less reliable than other fertility awareness approaches due to natural cycle variation.
Basal body temperature (BBT) tracking involves taking and recording body temperature daily upon waking to identify the temperature rise that occurs after ovulation. This method helps identify the infertile period after ovulation has occurred.
Cervical mucus observation involves monitoring changes in cervical secretions throughout the menstrual cycle to identify fertile and infertile periods. Fertile cervical mucus is typically clear, stretchy, and resembles raw egg white.
The symptothermal method combines multiple fertility indicators, including basal body temperature, cervical mucus changes, and other signs of ovulation to provide more accurate identification of fertile periods.
Ovulation Prediction
Ovulation predictor kits (OPKs) detect the surge in luteinizing hormone (LH) that occurs 24-36 hours before ovulation. These home test kits help identify the most fertile days of the cycle.
Fertility monitors are electronic devices that track multiple fertility indicators, including hormone levels, temperature, and other physiological changes to predict fertile periods with greater accuracy than single-indicator methods.
Mittelschmerz refers to ovulation pain experienced by some women mid-cycle, which can serve as an additional fertility awareness sign when combined with other indicators.
Emergency Contraception
Types of Emergency Contraception
Emergency contraceptive pills, also called morning-after pills, are hormonal medications taken after unprotected intercourse to prevent pregnancy. These medications are most effective when taken as soon as possible after unprotected sex.
Plan B One-Step contains levonorgestrel, a progestin hormone, and is available over-the-counter without age restrictions. It's most effective when taken within 72 hours of unprotected intercourse but may provide some protection up to 120 hours.
Ella (ulipristal acetate) is a prescription emergency contraceptive that may be more effective than levonorgestrel, particularly when taken 72-120 hours after unprotected intercourse.
The copper IUD can serve as emergency contraception when inserted within 120 hours (5 days) of unprotected intercourse. This method is the most effective form of emergency contraception and provides ongoing contraceptive protection.
Emergency Contraception Mechanisms
Emergency contraceptives primarily work by preventing or delaying ovulation, making fertilization less likely. They may also affect fertilization or implantation, though their primary mechanism is ovulation prevention.
Time sensitivity is crucial for emergency contraception effectiveness, with efficacy decreasing as time passes after unprotected intercourse. Seeking emergency contraception as soon as possible maximizes its effectiveness.
Permanent Contraception
Sterilization Procedures
Tubal ligation, commonly called "having tubes tied," is a surgical procedure that blocks or cuts the fallopian tubes to permanently prevent pregnancy. Various techniques are used, including cutting, burning, or blocking the tubes.
Tubal occlusion refers to non-surgical methods of blocking the fallopian tubes, such as the placement of small coils or plugs that cause scar tissue formation to block the tubes over time.
Vasectomy is a minor surgical procedure that cuts or blocks the vas deferens, the tubes that carry sperm from the testicles. This outpatient procedure is considered the safest and most cost-effective permanent contraception method.
Reversal and Considerations
Sterilization reversal involves surgical procedures to restore fertility after tubal ligation or vasectomy. Success rates vary based on the original sterilization method, time since the procedure, and individual factors.
Effectiveness of sterilization is very high, with failure rates less than 1% for most procedures. However, when sterilization fails, there's an increased risk of ectopic pregnancy, particularly after tubal ligation.
Fertility and Conception Terms
Basic Fertility Concepts
Fertility refers to the natural capability to produce offspring, influenced by age, health, genetics, and environmental factors. Fertility typically peaks in the early twenties and gradually declines with age.
Conception occurs when a sperm fertilizes an egg, typically in the fallopian tube. The fertilized egg then travels to the uterus for implantation and pregnancy development.
The fertile window encompasses the days during each menstrual cycle when pregnancy is possible, typically including the five days before ovulation and the day of ovulation itself.
Ovulation is the release of a mature egg from the ovary, typically occurring once per menstrual cycle around day 14 of a 28-day cycle, though timing varies among individuals and cycles.
Fertility Challenges
Infertility is defined as the inability to conceive after 12 months of regular unprotected intercourse for women under 35, or 6 months for women 35 and older. Infertility can affect men, women, or both partners.
Primary infertility refers to couples who have never been able to conceive, while secondary infertility describes difficulty conceiving after previously successful pregnancies.
Subfertility indicates reduced fertility that makes conception more difficult but not impossible, often requiring longer time or medical assistance to achieve pregnancy.
Assisted Reproductive Technology
In vitro fertilization (IVF) involves retrieving eggs from the ovaries, fertilizing them with sperm in a laboratory, and transferring the resulting embryos to the uterus.
Intrauterine insemination (IUI) places washed sperm directly into the uterus around the time of ovulation to increase the likelihood of fertilization.
Fertility medications stimulate ovulation or improve egg quality to enhance the chances of conception, either naturally or in conjunction with assisted reproductive procedures.
Pregnancy Planning and Preconception Health
Preconception Care
Preconception health encompasses steps taken before pregnancy to improve the likelihood of healthy conception and pregnancy outcomes. This includes optimizing nutrition, managing chronic conditions, and avoiding harmful substances.
Folic acid supplementation is recommended before conception and early pregnancy to reduce the risk of neural tube defects. The recommended dose is 400-800 micrograms daily for most women.
Preconception counseling involves healthcare consultations to assess and optimize health before attempting pregnancy, including reviewing medical history, medications, and lifestyle factors.
Pregnancy Testing and Confirmation
Human chorionic gonadotropin (hCG) is the hormone produced during pregnancy that is detected by pregnancy tests. HCG levels rise rapidly in early pregnancy and can be detected in urine or blood.
Home pregnancy tests detect hCG in urine and can provide accurate results as early as the first day of a missed period, though accuracy improves with time after the missed period.
Beta hCG blood tests measure exact hormone levels and can detect pregnancy earlier than urine tests while also monitoring pregnancy progression through rising hCG levels.
Family Planning Methods and Approaches
Reproductive Life Planning
Reproductive life plan involves thinking about and planning for if, when, and under what circumstances to have children throughout one's reproductive years. This planning helps guide contraceptive choices and preconception preparation.
Birth spacing refers to the time interval between pregnancies, with optimal spacing (18-24 months between births) associated with better health outcomes for both mothers and children.
Pregnancy intention describes whether pregnancies are planned, unplanned but wanted, or unwanted. Understanding pregnancy intention helps healthcare providers offer appropriate counseling and support.
Special Populations and Considerations
Adolescent contraception addresses the unique needs of teenagers, including considerations for confidentiality, side effects, ease of use, and effectiveness in preventing both pregnancy and STIs.
Postpartum contraception involves family planning immediately after childbirth, considering breastfeeding compatibility, timing of fertility return, and desired pregnancy spacing.
Perimenopausal contraception addresses contraceptive needs of women approaching menopause, when fertility declines but pregnancy remains possible until menstruation has stopped for 12 consecutive months.
Contraceptive Counseling and Decision-Making
Counseling Approaches
Contraceptive counseling involves healthcare discussions to help individuals choose the most appropriate birth control method based on their health, lifestyle, preferences, and reproductive goals.
Shared decision-making emphasizes collaboration between healthcare providers and patients in choosing contraceptive methods, ensuring that decisions align with individual values and circumstances.
Patient-centered care focuses on individual needs, preferences, and circumstances rather than provider assumptions about appropriate contraceptive choices.
Method Selection Factors
Efficacy considerations involve weighing the pregnancy prevention effectiveness of different methods against individual pregnancy prevention priorities and acceptable failure rates.
Side effect profiles describe potential adverse effects associated with different contraceptive methods, helping individuals make informed choices based on their tolerance for various side effects.
Reversibility refers to how quickly fertility returns after discontinuing a contraceptive method, important for individuals who may want to become pregnant in the future.
Cost considerations include both upfront costs and long-term expenses associated with different contraceptive methods, as well as insurance coverage and affordability programs.
Global and Cultural Perspectives
International Family Planning
Contraceptive prevalence rate measures the percentage of women of reproductive age who are using contraception in different populations, helping assess family planning program effectiveness and unmet need.
Unmet need for family planning describes women who want to avoid pregnancy but are not using effective contraception, highlighting gaps in contraceptive access and services.
Cultural competency in family planning recognizes how cultural, religious, and social factors influence contraceptive choices and reproductive decision-making across diverse populations.
Access and Equity Issues
Contraceptive access encompasses the availability, affordability, and acceptability of family planning services and supplies across different populations and geographic areas.
Health disparities in family planning describe differences in contraceptive access, use, and outcomes across racial, ethnic, socioeconomic, and geographic groups.
Reproductive justice frameworks connect individual reproductive choices to broader social, economic, and political factors that influence reproductive autonomy and health outcomes.
Understanding contraception and family planning terminology empowers individuals to make informed reproductive choices while facilitating better communication with healthcare providers and access to appropriate services. This knowledge serves as a foundation for reproductive autonomy and health throughout the reproductive lifespan.